Most patients with chronic pain will typically first be recommended a variety of pain medications and physical therapy, then once those fail, steroid injections, and then a joint surgery. Unfortunately, each step in this process is often ineffective at addressing the patient’s pain or creates a variety of complications that make their situation even more unbearable. For this reason, it is critical to understand the risks of each part of this process and the safer alternatives that can permanently alleviate joint and spinal pain.
Note: persistent or recurrent pain after spinal surgery, back pain following spinal surgery is referred to as “Failed Back Surgery Syndrome” and affects between 10-40% of people who receive a spinal surgery.
Common Spinal Pain Generators:
In most cases, joint pain has a cause that must be identified to treat it. For example, when treating spinal pain, we find it is critical to address:
- Tight muscles—rarely recognized despite being common (particularly of the iliopsoas and quadratus lumborum—two large and frequently tight muscle groups which directly attach to the lumbar spine). Physical therapists typically focus on strengthening rather than stretching/releasing tight muscles.
- Misalignment—requires adjustment and lifestyle corrections. A common cause of misalignment are uneven leg lengths which tilt the pelvis and hence the spine (and can be corrected with an appropriate heel lift).
- Ligamentous laxity—often the primary cause of spinal arthritis, muscle tightness, and disc problems as tight ligaments are necessary to ensure bones stay in the correct location and do not impinge tissues.
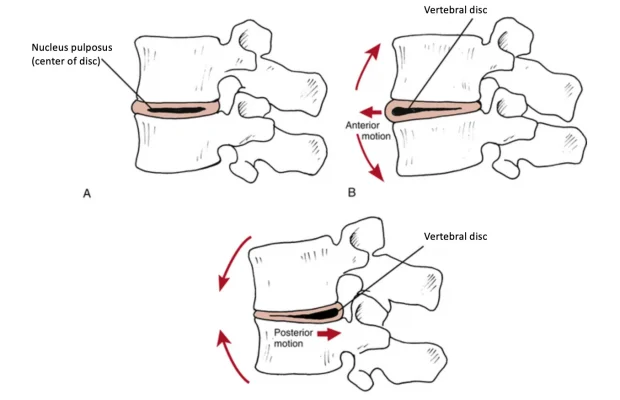
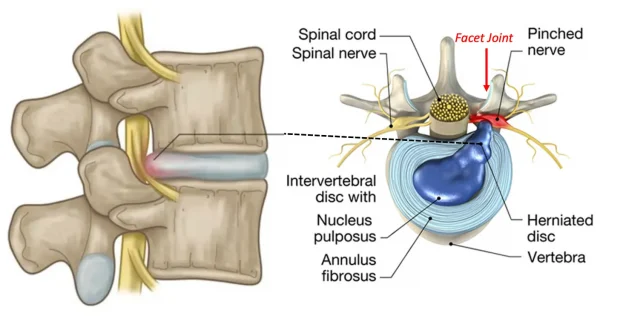
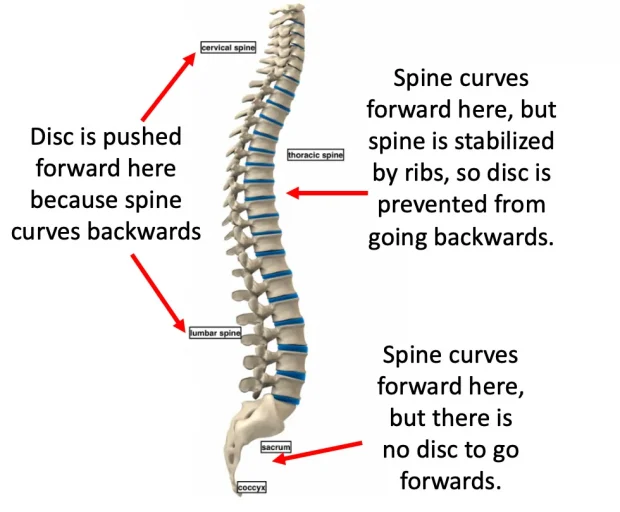
- Disc herniation—not the most common cause of back pain but sometimes a significant contributor (and frequently used as a justification for disastrous spinal surgeries). In most cases, disc herniations result from vertebrae bending too far forward, which pushes the discs back and compresses the nerves behind them.
- This can frequently result from a weakening of the spinal ligaments or poor posture which eliminates the natural backwards curve in the neck and low back.
- Note: tight muscles, joint misalignments, and ligamentous laxity also create issues in other regions of the body (e.g., the knees).
Additional Pain Generators:
- Trapped emotions: chronic stress and emotional distress frequently exacerbate pain (and in some cases are the primary cause of back pain). Dr. Sarno for example, addressed back pain through psychotherapy and generated a large following as his approach helped many (but not everyone).
Note: we frequently find a direct release of trapped emotions (rather than psychotherapy) is necessary to address chronic emotional trauma. - Nervous system dysregulation—over-activation of the sympathetic nervous system alongside under-activation of the parasympathetic system exacerbates pain.
Note: A common effect of unresolved trauma is fight-or-flight system over-activation. - Chronic inflammatory conditions (e.g., dietary allergies, mold toxicity, Lyme disease, spike protein injuries) often worsen pain patterns.
Note: many individuals have found that eliminating dietary food allergens resolves arthritis. - Scars from surgeries can frequently generate significant autonomic dysregulation and pain, and frequently, treatment of those scars yields dramatic improvements.
- Altered brain pain processing—often due to chronically over-activated nerves or microstroke injuring the thalamus (which otherwise dampens pain signals). In these instances, small stimuli can be extremely painful.
Systemic Medications
Since joint or spinal pain has multiple causes and diagnosis is time-consuming, physicians typically prescribe pills or refer patients elsewhere rather than address the root causes of their pain. Common medications include NSAIDs, Tylenol, Steroids, Gabapentin (or Lyrica), and Opioids—all with major issues.
Note: due to the high rate of addiction which follows opioid prescriptions (and the societal damage that follows), more and more, the government has moved to restrict opioid prescriptions. Because of this, patients in significant pain who will only respond to opioids, despite their best efforts, often cannot get these drugs and instead are given another ineffective option (e.g., NSAIDs), hence making it imperative that effective non-opioid solutions for pain be made available to the public.
NSAIDs
NSAIDs (e.g., ibuprofen, naproxen) temporarily reduce pain but only partially, leading patients to overuse them—often dangerously, as NSAIDs are toxic at high doses (which frequently occur since NSAIDs are taken for pain and are available over the counter). Many consider NSAIDs among the most hazardous drugs in the U.S. because:
- They are the leading cause of drug-related hospital admissions—often due to heart attacks, strokes, bleeding, and kidney failure.
- Kidney damage is a significant risk. One study found a 20% increased risk of kidney disease from NSAIDs; others found up to 212%. Amongst kidney failure patients, 65.7% were found to be chronic NSAID users.
- NSAIDs raise cardiovascular risks. NSAIDS also increase the risk of heart attacks and death (e.g., extensive studies have found between a 24-326% increase1,2,3). Two of the worst ones, Vioxx (Merck) and Celebrex (Pfizer), were designed to reduce stomach bleeding but instead caused heart attacks and strokes. Merck hid data on Vioxx’s risks; eventually it was withdrawn after an estimated 120,000 deaths. Celebrex, still on the market, has been linked to 75,000 deaths. Merck’s handling of Vioxx later informed how pharma pushed the HPV vaccine and mRNA vaccines.
- Gastrointestinal bleeding is common and often fatal. In 1999, over 16,000 Americans died from it. NSAIDs also cause small bowel damage in over 50% of chronic users—often undetected—leading to “small bowel enteropathy” and possibly chronic illness through gut permeability.
- They impair healing, especially of ligaments, creating long-term re-injury risk.
Trials alleging the benefit of NSAIDs are frequently intentionally deceptive and frequently create the illusion of a benefit where none exists. What this means is that many patients ruin their lives with drugs that did almost nothing for them in the first place.—Peter Gøtzsche
Unfortunately, NSAIDs remain amongst the most commonly prescribed drugs, and are frequently given for musculoskeletal injuries.
Note: the dangers of NSAIDs are discussed further here.
Tylenol
Tylenol (acetaminophen) is one of the few over-the-counter alternatives to NSAIDs and is generally considered safer, though often ineffective for severe pain. Still, it carries serious risks:
- Liver Toxicity: Overuse leads to 56,000 ER visits, 2,600 hospitalizations, and 500 deaths annually in the U.S. due to Tylenol toxicity.
- Fever Suppression: Tylenol reduces fevers, which are key immune defenses. Suppressing them can worsen or prolong infections—a pattern observed during COVID-19. Many parents of vaccine-injured children reported symptoms (e.g., autism) appeared after using Tylenol to suppress high post-vaccine fevers, explored in this 2021 paper.
Gabapentin and Pregabalin
Gabapentin (Neurontin) was originally approved to treat epilepsy—a small market. After approval, Pfizer aggressively pushed it for unapproved uses, especially neuropathic pain, despite limited evidence. The federal government fined Pfizer nearly $1 billion for illegal promotion.
While less toxic than NSAIDs, side effects for these drugs are common and include: lethargy, dizziness, sedation, and cognitive impairment, as well as rarer but serious reactions like respiratory depression and hypersensitivity. Gabapentin can also be habit forming.
Note: since gabapentin and pregabalin (Lyrica) only work for specific types of pain (e.g., neuropathic pain), they typically do very little for most patients’ pain. However, they are widely prescribed because they lack many of the severe risks associated with other pain reducing drugs, and as a result, many are placed on inappropriate prescriptions for them.
Corticosteroids
Initially hailed as a wonder drug, corticosteroids like prednisone and hydrocortisone gradually were discovered to have significant side effects (e.g., weight gain, adrenal suppression, heart attacks, diabetes, insomnia, and psychiatric effects). Since corticosteroids trigger tissue breakdown, they also often greatly weaken the body’s structural integrity, impair wound healing and weaken collagen synthesis.
Furthermore, corticosteroids double one’s risk of fracture (especially vertebrae), with 12% of users reporting fractures. Steroids cause 5-15% bone loss yearly, and 37% of long-term users experience vertebral fractures. High doses increase vertebral fracture risk fivefold. Higher doses also cause avascular necrosis in 6.7% of users. Likewise, they greatly impair wound healing, collagen
Note: the primary drugs used to treat Osteoporosis (bisphosphonates) have severe side effects have severe side effects including making the bones more likely to break. In turn, one of the few approved uses for bisphosphonates is steroid-induced bone loss.
Since both collagen, ligaments (which are composed of collagen) and bones are weakened by steroids, chronic use leads to joint weakening and chronic pain. Because of this, we frequently encounter patients who achieved a temporary alleviation of joint pain (e.g., in the spine or knee) who then have their condition worsen and require surgery. Unfortunately, this side effect is rarely disclosed to patients, leading to many surgeries that could have been prevented.
Note: in many cases, if joint pain is instead treated by strengthening the ligaments (e.g., with nutritional supplementation or prolotherapy), the pain will resolve and future surgeries can be prevented.
The Surgery Funnel
Surgeries often have risks that patients don’t learn about until after complications occur, which is problematic since you can’t “undo” surgery. For this reason, patients should seek unbiased second opinions from doctors who aren’t being paid to do a proposed surgery.
Unbearable pain (e.g., in a joint) is one of the strongest motivators for surgery, and spinal surgeries are the most common elective surgery I’m consulted about. Unfortunately, since spinal surgeries are one of the most profitable areas in medicine, there’s reluctance to consider if risks outweigh benefits or if safer and more effective alternative exist, and over the years I’ve become increasingly skeptical of them, as while some are necessary and help patients, many are not.
Likewise, despite trillions spent on spinal pain (e.g., in 2016, 134.4 billion dollars was spent on neck and low back pain in the USA), most patients remain stuck with chronic pain and experience significant side effects from treatments.
Note: there have been numerous newspaper investigations of spinal surgeons who recklessly performed large volumes of unnecessary surgeries, killing or injuring many of their patients who were nonetheless protected by their hospitals because of how much revenue they generated.