Six weeks ago, President Trump was scheduled to give remarks on the potential causes of autism. Shortly beforehand, the press became aware that Trump would focus on the link between Tylenol and autism, resulting in the national media collectively ridiculing that link immediately before the press conference.
In that press conference, Trump stated he had felt very strongly about bringing attention to vaccines and autism for 20 years, that he felt we were giving too many shots too quickly, and that they needed to be spaced out. There was no reason to give the hepatitis B vaccine prior to children being 12 (which, as I showed here, is true), and Tylenol increases the risk of autism, so if possible, it should be avoided during pregnancy, and you should not give it to infants.
Secretary Kennedy added that some 40 to 70% of mothers who have children with autism believe a vaccine injured their child, and that President Trump believes we should be listening to these mothers instead of gaslighting them—something many of us never expected we would hear in our lifetimes from the Federal government.
Note: regrettably, to show they believed in “Science”, pregnant mothers began quickly posting videos of themselves taking large amounts of Tylenol (which I compiled on here—including a tragic overdose).
Over-the-Counter Pain Management
Because of how uncomfortable pain is, pain treatments have long been a core market in medicine. Remarkably however, most standard pain therapies have serious issues and often lead patients to needing more and more severe interventions.
Typically, the first-line treatment for pain is an over-the-counter medication, such as acetaminophen (Tylenol), ibuprofen (Advil or Motrin), naproxen (Aleve), aspirin, or topical diclofenac (Voltaren gel). Unfortunately, these medications all have dose-dependent toxicity and typically only elicit partial improvement in pain.
Many consider NSAIDs (ibuprofen and naproxen) amongst the most hazardous drugs in the U.S. because:
• They are the leading cause of drug-related hospital admissions—often due to heart attacks, strokes, bleeding, and kidney failure (e.g., at least 107,000 Americans are admitted to hospitals each year for NSAID GI bleeds).
• Kidney damage is a significant risk. One study found a 20% increased risk of kidney disease from NSAIDs; others found up to 212%. Amongst kidney failure patients, 65.7% were found to be chronic NSAID users.
• NSAIDs raise cardiovascular risks. NSAIDS also increase the risk of heart attacks and death (e.g., extensive studies have found between a 24-326% increase1,2,3). Two of the worst ones, Vioxx (Merck) and Celebrex (Pfizer), were designed to reduce stomach bleeding but instead caused heart attacks and strokes. Merck hid data on Vioxx’s risks; eventually it was withdrawn after an estimated 120,000 deaths. Celebrex, still on the market, has been linked to 75,000 deaths. Merck’shandling of Vioxx later informed how pharma pushed the HPV vaccine and mRNA vaccines.
• Gastrointestinal bleeding is common and often fatal. In 1999, over 16,000 Americans died from it. NSAIDs also cause small bowel damage in over 50% of chronic users—often undetected—leading to “small bowel enteropathy” and possibly chronic illness through gut permeability.
• They impair healing, especially of ligaments, creating long-term re-injury risk.
Note: the dangers of NSAIDs are discussed further here.
The poor efficacy of OTC pain medications, along with their significant toxicity, was one of the primary reasons I spent the last year trying to bring attention to DMSO, which is dramatically more effective than any other over the counter option (e.g., I compiled extensive literature demonstrating that here, and have received well over a thousand reports from readers saying it produced miraculous improvements in pain)—and more more importantly does not have the major safety issues seen with most over the counter pain killers.
Note: I am currently working on an article about DMSO’s uses for genitourinary conditions (e.g., menstrual or prostate issues, infertility, erectile dysfunction, UTIs or cystitis). If you have had any DMSO experiences with them you can share (e.g., by replying to this), that would greatly help the readership here.
Tylenol Toxicity
Tylenol (acetaminophen or paracetamol) is generally considered safer than NSAIDs, though it too is often ineffective for severe pain. When metabolized, it produces the metabolite NAPQI (N-acetyl-p-benzoquinone imine), which is highly toxic to liver cells because it irreversibly binds to essential cellular proteins.
Typically, relatively little NAPQI is produced and is quickly neutralized by liver glutathione. However, when too much Tylenol is taken, the other detoxification pathways get saturated, glutathione stores get used up, and rapid liver death from unneutralized NAPQI ensues.
As a result, Tylenol overuse leads to 56,000 ER visits, 2,600 hospitalizations, and 500 deaths annually in America.
Additionally, Tylenol has several other major issues:
• NAPQI is also toxic to the kidneys, and in 1-2% of overdose cases, the kidneys are also damaged.
• Numerous studies have linked gastrointestinal side effects to the use of Tylenol.
• In one review, Tylenol was found to increase the risk of: bleeding or perforated peptic ulcers (+6–121%), heart failure (+9–98%), myocardial infarction (+0–73%), hypertension (+7–62%), and chronic renal failure (+19–129%).
• A systematic review identified data suggesting chronic Tylenol use increased blood pressure, increased asthma (a possible 15% increase), and caused a 3.6-3.7 increase in gastric bleeding.
• Tylenol has been associated with an increased risk of blood cancers: +16% from low use and +84% from high use.
• In children of mothers chronically using Tylenol, a review found the following increases: hyperkinetic disorder (+37%), ADHD medication use (+29%), autism spectrum disorder with hyperkinetic symptoms (+51%), and asthma in offspring from frequent use in late pregnancy (+110%).
• A recent systematic review of 46 studies conducted on the risk of Tylenol during pregnancy causing neurodevelopmental disorders (NDDs) in offspring found that the majority of studies detected an increased risk, those of higher quality were more likely to detect the association, and the increase was dose-dependent. The increased NDDs included autism, ADHD, and other NDDs affecting learning, social/motor skills, attention, cognition, emotions, and behavior.
Note: this study is arguably the most definitive proof that Tylenol is not safe during pregnancy and was the one Trump and RFK’s team highlighted at their recent vaccine announcement.
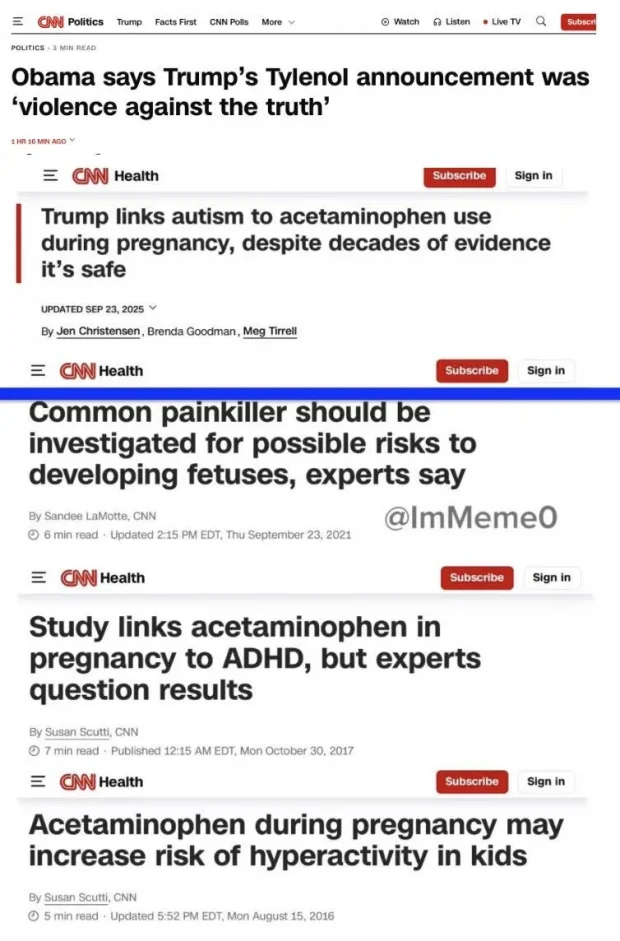
All of this led to a rather peculiar media phenomenon:
Note: numerous internal documents and public statements have shown that by 2017, Tylenol’s manufacturer was well aware of the drug’s link to autism.
Treating Fevers
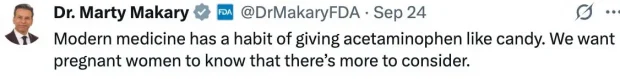
A standard hospital procedure is for nurses to check patients’ vital signs every few hours, and if anything is abnormal, contact the supervising doctor. One of my continual challenges was telling nurses I did not want to treat fevers—something which doctors had diametrically opposed views on, with the majority wanting to treat fevers. I was quite astonished to see the head of the FDA speak out against this practice:
Why Do We Treat Fevers?
There are a few justifications for treating fevers:
1. Fevers significantly increase metabolic demand on the body, placing additional stress on vital organs. In ICU settings where organ functions are compromised, reducing metabolic demand may prolong survival—though it’s acknowledged that fevers aid in eliminating infections. There is no clear consensus within critical care on how fevers should be managed.
Note: Ultraviolet Blood Irradiation, a potent therapy for infectious diseases that also treats a variety of other conditions and often appears to “re-energize” the body, as a myriad of poorly functioning systems resume their normal function during a UVBI session. I mention this as one of the primary “side effects” of UVBI is that when it eliminates an infection it will often create a fever.
2. High fevers can cause brain damage. Hyperpyrexia is defined as a medical emergency, with thresholds ranging from 105.8°F to 106.7°F. According to Penn State, brain damage generally won’t occur unless the fever exceeds 107.6°F.
3. In children, fevers can sometimes lead to seizures. However, a 2017 Cochrane review found that fever-reducing medications provide no benefit for preventing febrile seizures, and the American Academy of Pediatrics recommends against this practice.
4. To reduce the discomfort of the fever (the primary reason most Tylenol is prescribed).
Arguments Against Treating Fevers:
1. Fevers provide valuable diagnostic information about new or recurring infections.
Note: in infants, unexplained fevers over 100° often warrant a (justified) immediate evaluation for sepsis—which is one of many reasons why the (fever-causing) newborn hepatitis B vaccine is so problematic.
2. Relapsing fevers characterize certain autoimmune and infectious diseases, so, if a fever is artificially suppressed, the diagnostic signal is lost.
3. The body relies upon fevers to eliminate illness, and in some trials, suppressing fevers extends the duration of illness.
4. As Tylenol has systemic toxicity and reduces liver function and glutathione (necessary to detoxify toxins), this can potentially worsen certain illnesses or increase the likelihood a vaccine will cause autism.
5. Suppressing febrile illnesses transforms them into more severe infections.
Of these, the fifth is the least appreciated and hence will be expanded upon.
The 1918 Influenza
In December 2019, I became aware of COVID-19 and became very worried that it would cause serious problems. We spent January and February studying a variety of resources, including literature from the 1918 pandemic that provided critical insights for treating COVID-19 (and saved the lives of those in our close circle).
Note: I consider the 1918 influenza pandemic one of the most deadly and devastating pandemics in history. Over 2.5% of those infected died (with much higher rates ranging from 12%-90% in Native American populations). Since most of the treatments tried failed, the few that worked were quite noteworthy to me.
Throughout that literature, many clinicians treating the infection stated that using aspirin on patients’ fevers significantly increased their risk of dying and that those who had previously been treated with aspirin tended to have the poorest response to the therapies, which otherwise worked for the illness.
Note: at that time, doctors routinely used large aspirin doses which are known to be toxic.
Since that time, fevers have been recognized as critically important in fighting infections. Some of the key pathways include:
- Fevers boost the activity of immune cells like neutrophils, monocytes, and T-cells
- Fevers promote type I interferon responses that inhibit viral replication
- Fevers trigger heat shock proteins to activate immune defenses
- Fevers work synergistically with stressors like iron deprivation to amplify damage to pathogens
- Fevers slow pathogen growth early, helping to control infections
During COVID, I had multiple conversations with people where I advised them against suppressing fevers with Tylenol or ibuprofen. Still, they did anyway, then decompensated and had to go to the ER. I found that heating someone who was acutely ill (particularly with infrared mats) often made them feel significantly better immediately, and no longer want fever medication. From this, I formed the hypothesis that the discomfort associated with fevers results not from the heat itself, but rather from the strain the body undergoes in trying to heat itself.