On Monday, the Trump administration carried out the most significant weakening of federal vaccine guidance in modern public health history, slashing the number of diseases the childhood vaccine schedule recommends routine vaccination against from 17 to 11. The move came less than 30 days after President Donald Trump issued an unusual directive, tasking officials with determining if the United States’ schedule should resemble countries with fewer routine shot recommendations, namely Denmark.
Two skeptics of the COVID vaccine, who were appointed to administration roles just last month, authored a brief assessment justifying the overhaul. Jim O’Neill, the acting director of the Centers for Disease Control and Prevention (CDC), quickly authorized the changes to the schedule.
Now, vaccination against hepatitis A, hepatitis B, meningitis, respiratory syncytial virus (RSV), influenza, and rotavirus are no longer recommended for all children. The rollback was crafted behind closed doors with no public discussion or debate and no input from the federal advisory committee that has voted on vaccine recommendations to the CDC at public meetings for decades.
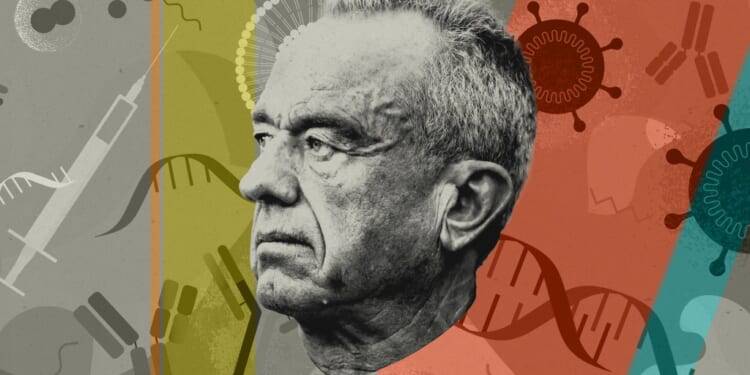
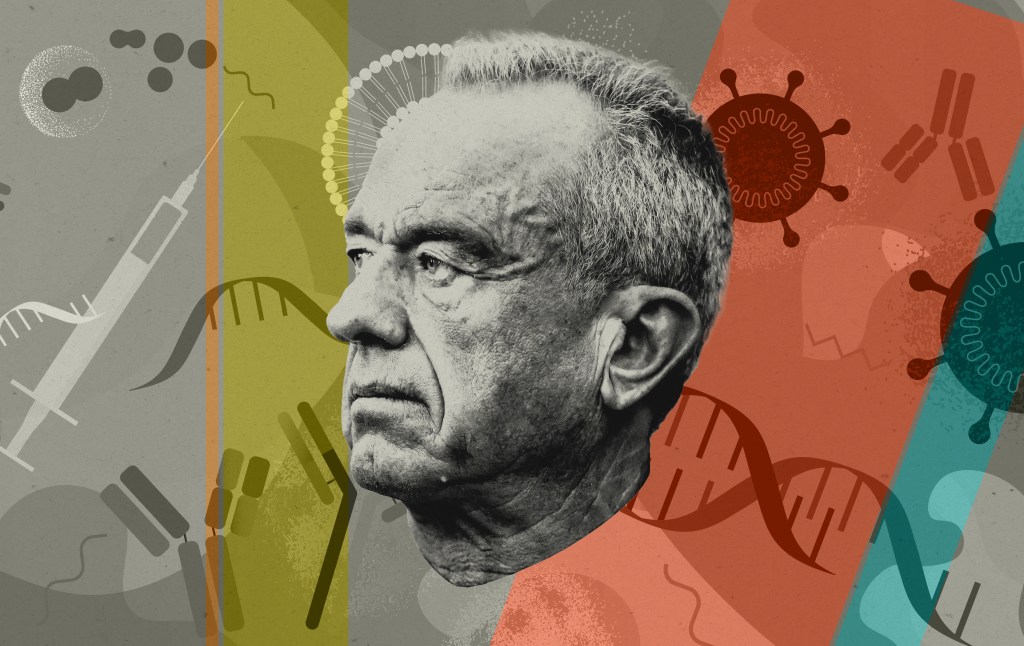
The move marks the culmination of Robert F. Kennedy Jr.’s campaign as Health and Human Services secretary to bend the federal immunization guidance to his long-held vaccine-skeptical views.
Contradicting his commitments.
It’s worth reviewing the past 11 months of Kennedy’s leadership at HHS to understand how inconsistent this week’s actions are with the secretary’s previous statements and promises about his plans, both before and after the Senate confirmed him.
Kennedy pledged in his confirmation hearing that he wouldn’t make changes to the childhood vaccine schedule, and GOP Sen. Bill Cassidy, a physician and the lawmaker who cast the key vote advancing the secretary’s nomination, said Kennedy told him the federal advisory committee responsible for making recommendations to the CDC on the vaccine schedule would be maintained without changes. Kennedy also said he wouldn’t insert himself into scientific determinations about vaccines.
The secretary quickly reneged on the commitments. In May, Kennedy unilaterally rescinded the COVID-19 vaccine recommendations for pregnant women and children. The next month, he fired all 17 members of the Advisory Committee on Immunization Practices (ACIP) over unsubstantiated allegations of corrupt conflicts of interest. He then packed ACIP with allies and vaccine skeptics, several of whom had conflicts of interest themselves. The new body quickly went about sidelining career CDC scientists and external advisers while platforming figures who have built careers in the anti-vaccine movement. Over the course of several chaotic meetings that featured confusion among members about the committee’s authority and the actual effects of its actions, the body rolled back longstanding recommendations, including ending the universal hepatitis B birth dose recommendation and removing a recommendation for the combined measles, mumps, rubella, and varicella (MMRV) vaccine for younger children.
Kennedy fired the administration’s own pick for CDC director, Susan Monarez, who said her ouster came after she told the secretary she wouldn’t preemptively rubber-stamp ACIP’s recommendations. The revelation suggested the committee was no longer functioning as an independent source of guidance but doing Kennedy’s bidding. Still, the secretary insisted that vaccine decisions remained independent. At the committee’s most recent meeting last month, the ACIP chair was caught on a hot mic saying he felt like a puppet on a string.
Public health researchers and scientists decried what they saw as a supplanting of transparent and evidence-based decision-making in favor of rote skepticism from people unqualified to understand vaccine science, let alone recommend changes to the schedule. But Kennedy and his allies could still claim they were operating within the rules and structure of the recommendation system, not acting as ideologues circumventing ACIP.
This week’s truncating of the schedule removed whatever pretense remained that Kennedy’s HHS would respect the scientific process for making decisions about vaccines even when that process was dominated by allies who had already taken action to roll back recommendations.
Former ACIP members explain that an adjustment to a single vaccine recommendation would previously have taken months of work, if not a year. ACIP members and CDC scientists would go through lengthy systematic reviews of evidence and also seek input from outside doctors and other stakeholders who would be affected by any change. Dr. Kevin Ault, the vice president of the National Foundation for Infectious Diseases who served on ACIP when it expanded the adult hepatitis B recommendation to be universal in 2022, told The Dispatch that this week’s changes normally would have required years of study and review. “It would have involved input from people on the ground,” Ault added. “That type of input is being ignored.”
These are “historic wholesale revisions to the schedule made at the stroke of a pen, but more importantly, in a matter of a few weeks, by a few individuals writing a few memos,” said Jason Schwartz, a professor at the Yale School of Public Health who researches vaccine policymaking. “It’s just light years away from anything we would have expected for decades regarding vaccine policymaking in the U.S.”
“Clearly, this group just does not believe that the federal government should be exhorting individuals to get vaccines,” he added.
The Denmark model and a faulty consensus.
Dr. Tracy Beth Høeg, a sports medicine physician whose work and research largely focused on marathon runners until she became a critic of the COVID-19 public health response, and Martin Kuldorff, an epidemiologist who co-authored the Great Barrington Declaration criticizing pandemic lockdowns, wrote the 33-page assessment behind the schedule change, arguing the U.S. is an outlier among rich countries in the number of diseases the childhood schedule recommends universal vaccination against.
The assessment includes a data table listing 20 “peer nations” and uses the group to argue that the American schedule goes beyond “consensus vaccines” in recommending childhood immunization against 17 diseases—not counting the recommendation for monoclonal antibody treatment to protect infants against RSV.
The report doesn’t define what is meant by peer nations, aside from rich and developed, or explain why this particular group makes for an appropriate analog to the U.S. The stated model for the new schedule is Denmark, a country that recommends universal childhood vaccination against only 10 diseases. Out of the 20 peer nations considered in the report, Denmark doesn’t jump off the page as an especially good comparison. The Danish population is ethnically homogeneous and 6 million strong, roughly the size of the Atlanta metro area. The country has a universal health care system and a centralized, national registry to keep track of patients.
It’s unclear why Denmark is the better “peer” model than our northern neighbor, Canada, which recommends universal childhood vaccination against 15 diseases, or Japan, a country of more than 120 million people that targets 14 diseases. Infectious diseases researchers and current and former CDC officials have argued the U.S. doesn’t necessarily have a peer nation from a public health perspective, given the unique structure and gaps of the American health care system and the size and health disparities of the U.S. population.
But taking the report’s presentation of peer nations at face value, it’s not statistically true that the U.S. is an outlier in the number of universal vaccine recommendations, at least not as much of an outlier as Denmark. According to the included table, in 2024, the U.S. schedule targeted 17 diseases, the most out of the group, but the median number of recommendations among the 20 nations is 14; the average is 13.6. Denmark’s 10 is the fewest on the list—no other country in the group recommends fewer than 12. The shift to universal vaccination against just 11 diseases leaves the U.S. schedule numerically as far below the median as it was previously above the median. The changes don’t move the U.S. more toward the middle but second to the bottom.
Why are officials focusing on Denmark in the first place? It seems that Høeg just really likes Denmark. She spent years living there while pursuing her Ph.D., married a Danish man, and became a dual citizen.
But it turns out that even Danish health officials don’t understand why the U.S. would try to outsource its recommendations. “Personally, I do not think this makes sense scientifically,” Anders Hviid, an official in Denmark’s Statens Serum Institute, which is part of the country’s ministry of health, told the Washington Post. “Public health is not one size fits all. It’s population specific and dynamic. Denmark and the U.S. are two very different countries.”
“It is surreal, and it is difficult, from a Danish perspective, to understand what’s going on,” he added.
The idea of “international consensus” vaccines also doesn’t seem to hold water, according to Høeg and Kuldorff’s own selection of peer countries. They claim that “several vaccines currently included in the childhood immunization schedule in the U.S. (hepatitis A, varicella, influenza, rotavirus, and meningococcal vaccines) are limited in their recommendation or excluded in some other developed countries.” That’s true for hepatitis A and influenza. But according to the report, the rotavirus vaccine is universally recommended by 17 of the 20 peer countries. Denmark is one of just three that omit the immunization. Fifteen of 20 also include universal recommendations for meningococcal vaccines, and 18 of the 20 peer nations have universal recommendations for hepatitis B.
To be clear, Høeg and Kuldorff argue that the U.S. should follow the consensus vaccines of a group of countries they selected themselves, but their new schedule leaves out multiple universal recommendations that the overwhelming majority of the group actually includes.
Their “consensus” doesn’t appear to represent an actual consensus, but it does function as a convenient rhetorical device, and the focus on peer nations was reportedly useful for Kennedy and his aides in pushing the White House to support the shift.
Implications of the new schedule.
Vaccinations against four diseases—RSV, hepatitis A and B, and meningitis—are now recommended as routine for certain “high-risk” groups. For populations that aren’t considered high risk, the CDC now recommends that the decision to vaccinate against the four diseases be made in consultation with a health care provider, a designation called “shared clinical decision-making” (SCDM) that essentially signifies immunizations the CDC doesn’t believe are beneficial for all children and are often viewed as optional by patients. Vaccines against rotavirus and influenza, previously recommended for all children, are listed only under this category and not encouraged for any high-risk groups. The human papillomavirus vaccine (HPV) recommendation remains universal, but the number of recommended doses has been reduced from two to one.
HHS officials have said that the narrowing of guidance for vaccines that were previously recommended for all will not affect coverage under the Vaccines for Children Program, which subsidizes vaccines for uninsured or underinsured families, or requirements that private insurance cover those vaccines at no cost. But doctors have argued that shifting recommendations from universal to SCDM can still undermine access even if coverage remains unchanged.
“Routine recommendations establish defaults,” said Dr. Jake Scott, an infectious disease physician and researcher at Stanford University. “They trigger automatic prompts in electronic health records. They shape what providers discuss and when. They send a signal about what the weight of evidence supports. Critically, they enable standing orders, the protocols that allow nurses and pharmacists to vaccinate without a specific physician examination or direct order for each patient. Shared decision-making voids all of this.” Kennedy’s May rescission of COVID vaccine recommendations resulted in confusion among providers, and many people were initially unable to get vaccines at pharmacies without a doctor’s prescription.
“The playbook is now clear: invoke shared decision-making not as a scientifically grounded response to genuine uncertainty but as a mechanism for stepping back from vaccines without formally withdrawing them,” Scott said. “It creates the appearance of patient autonomy while erecting structural barriers to care. It uses the language of nuance to accomplish blunt ideological goals.”
In an interview with CBS News correspondent Nancy Cordes on Wednesday, Kennedy seemed to acknowledge the new schedule could make vaccine access more difficult. Cordes asked if the changes would make it harder for parents to get a flu shot for their kids at pharmacies. “So, fewer people will get the flu vaccine,” Cordes suggested.
“Well, that may be, and maybe that’s a better thing,” Kennedy replied.
Chances of a legal challenge.
Dorit Reiss, a law professor at the University of California-San Francisco whose work focuses on vaccine legal issues, told The Dispatch the schedule overhaul could face legal scrutiny because it sidelined ACIP. While ACIP is an advisory body established at the prerogative of an executive agency rather than by statute, its role in vaccine recommendations is referenced in several laws, including the Affordable Care Act. Reiss said that the absence of the usual procedure with the schedule change as well as the relatively limited explanation officials provided in supporting documents could potentially run afoul of the Administrative Procedure Act’s “arbitrary and capricious” standard.
Medical associations sued to challenge Kennedy’s changes to COVID vaccine guidance and ACIP firings last year on these grounds. Schwartz, the vaccine policy researcher, said he thinks this week’s changes are more likely to withstand legal scrutiny since officials provided at least some rationale, in contrast to Kennedy’s one-page directive in May. He did add that the shift from recommending two doses of the HPV vaccine to one could potentially provide a basis for a stronger challenge since the official explanations only address it in a few sentences.
Even if a lawsuit succeeded, it’s unclear how much of a dent it would make in the administration’s message that there’s insufficient evidence that vaccines are safe and that parents should have their children receive fewer of them. “Ultimately, so much of what these recommendations boil down to is what the government is saying about the importance of vaccines,” Schwartz said. “And there isn’t a lawsuit that will change the sentiments and statements that we’re seeing from our health officials when it comes to vaccines.