Introduction
In an effort to restrain the growth of health-care spending, policymakers have attempted to fund the highest-quality care at the lowest cost. But this funding model poses a challenge for rural hospitals, which have high fixed costs spread over small patient populations.
The federal government has tried to support small rural hospitals by allowing them to charge 84% more for inpatient procedures delivered to Medicare patients. But rural residents increasingly prefer to travel to receive care from urban hospitals, which offer more specialized physicians, cutting-edge equipment, and better treatment outcomes—at lower cost.
Congress recently opted for a better approach, by offering small rural hospitals lump-sum payments of $3 million per year each to maintain essential emergency care, regardless of inpatient numbers. But even with these payments, weak administrative capacity and poor access to capital have made it hard for rural hospitals to restructure to a focus on emergency care. In order to support the transition, Congress should permit isolated rural hospitals to claim three years of lump-sum payments up front, in return for a five-year commitment to provide emergency care.
The Rural Health-Care Challenge
Efficient hospital care requires substantial economies of scale, which makes it difficult for rural facilities to compete on cost or quality of care.
In 2020, 20% of the U.S. population lived in rural areas,[1] which are home to 49% of the nation’s hospitals but only 10% of its physicians.[2] Nonmetropolitan counties had an average of 13 physicians per 10,000 residents, compared with 31 in metropolitan counties.[3]
Rural residents have distinct and significant medical needs: they are slightly older (18% over the age of 65) than those in urban areas (14%) and have a 26% higher age-adjusted mortality than those living in major metro areas.[4] The average income of isolated rural communities was 15% lower than in urban areas.[5] Patients in nonmetropolitan areas had significantly higher mortality rates for heart disease, stroke, cancer, injury, and respiratory disease.[6]
Despite these health issues, rural residents generally enjoy good access to care. Rural patients are more likely to have a regular source of medical care than those in urban areas, and they have a similar overall rate of unmet health-care needs. Rural patients face similar waits and travel times to receive primary care as those in urban areas.
But some types of care are harder to access in rural areas. To see a specialist, rural residents face longer waits and must travel twice as long.[7] Rural Medicare beneficiaries use a third fewer health-care services than those in urban areas—largely because of fewer encounters with specialty physicians. They use a similar amount of inpatient and post-acute hospital services but are more likely to receive outpatient services in a hospital setting.[8]
Rural areas are served by a large number of very small hospitals. In 2019, 1,805 of the country’s 5,141 community hospitals were located outside metropolitan areas.[9] While urban hospitals average 1,517 full-time employees, rural hospitals average only 321, which drops to only 138 in isolated rural areas.[10] In urban areas, the average hospital bed occupancy rate is 62%, compared with 37% in rural hospitals.[11] Whereas the median hospital patient census in urban hospitals is 102, in rural facilities it is 7, and in isolated rural communities it is only 2.[12] Small rural facilities account for 25% of U.S. hospitals but only 2% of hospital spending.[13]
Most small rural hospitals deliver emergency care, inpatient services, laboratory tests, and rehabilitation.[14] A total of 86% of rural hospitals offer surgical care (vs. 97% in urban areas), and 58% offer obstetric services (vs. 72%) but are less likely to have chemotherapy (49% vs. 84%), intensive-care units (46% vs. 82%), or psychiatric units (16% vs. 34%).[15] Most (72%) also have “swing beds,” which can be used for either acute care or long-term care.[16]
Rural hospitals generally lack the most expensive equipment because of the economies of scale involved in hospital care. A total of 84% of hospital expenditures are fixed costs, which do not vary directly with the number of patients treated.[17] Large patient populations are needed to spread the costs of specialized physicians and capital investments over many cases. Maximum hospital efficiency requires about 200 patient beds, while most rural hospitals have fewer than 25.[18] As a result, rural hospitals are less likely to have costly intensive-care units, cardiac catheterization labs, or robotic surgery.[19]
The quality of surgery is often worse at low-volume hospitals.[20] As one stakeholder remarked rhetorically: “Do you want your gallbladder taken out in a place that does two of them a year?”[21] Heart surgery performed at low-volume facilities had more complications, higher mortality, and higher cost.[22] Patients receiving knee replacements at low-volume hospitals had worse functional outcomes.[23] Emergency-room mortality was also higher at low-volume hospitals, with the largest difference associated with sepsis.[24] Patients with heart attacks, strokes, and pneumonia in rural hospitals were much less likely to receive appropriate treatment and suffered higher rates of mortality.[25]
Rural hospitals face less local competition than urban facilities, but rural residents nonetheless often travel to obtain surgical procedures from larger urban hospitals with higher quality and lower cost. In 2018, rural Medicare beneficiaries obtained 40% of inpatient procedures from facilities other than the one nearest their home—88% of which could have been performed at the nearer facility.[26] Patients seeking complex procedures, or enrolled in managed care, were more likely to receive surgery from distant hospitals.[27] Even if patients do not choose to travel, rural hospitals are less likely than their urban counterparts to admit patients for the same conditions and more likely to transfer them to other facilities.[28]
Rural hospitals have lower occupancy rates and are typically less profitable. Whereas the average profit margin at urban hospitals was 5.4% in 2023, it was only 3.1% at rural facilities—39% of which lost money.[29] From 2008 to 2018, half of unprofitable rural hospitals returned to profitability, 17% merged with other facilities, and 7% closed their doors.[30]
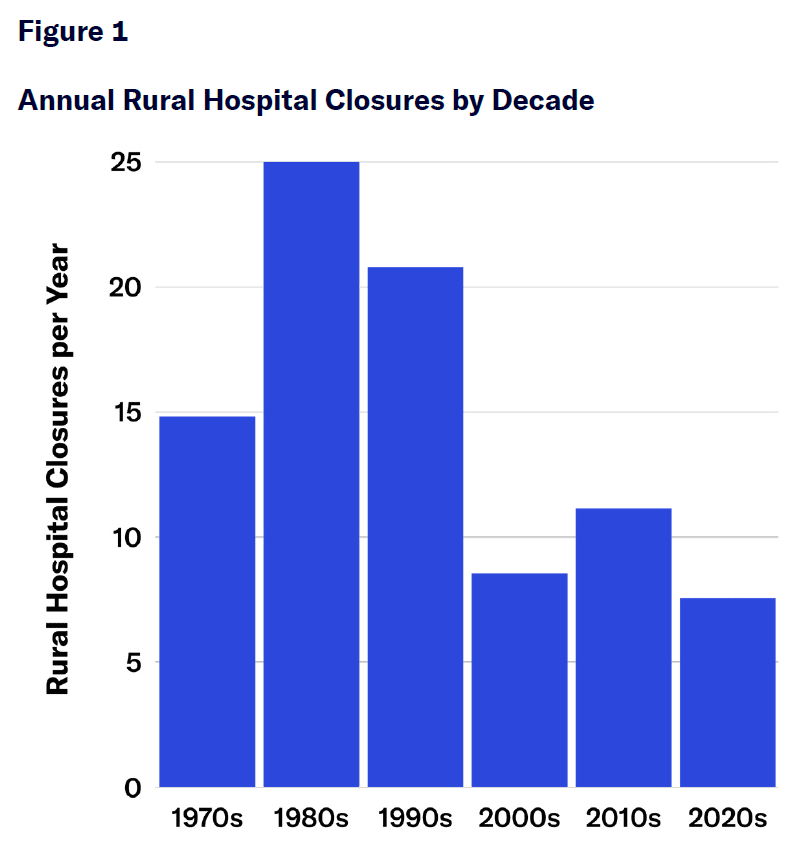
Since 1970, more than 800 rural hospitals have closed (Figure 1). Hospitals that closed tended to be small facilities in competitive markets serving declining local patient populations, with persistent losses and no financial support from local government.[31] Hospital closures tended to be preceded by more substantial declines in impatient admissions, with patients increasingly bypassing these facilities for distant alternative sources of care.[32]
Hospital closures eliminate fixed costs and reduce average costs at surviving hospitals. Closures increase the likelihood of nearby facilities performing surgery by 50% because of increased demand and relaxation of workforce supply constraints. Nearby facilities see their nursing staff increase significantly following closures.[33] Outpatient visits tend to shift from hospitals to other settings, such as physician offices, following closures.[34]
Childbirth is the most common reason for hospitalization.[35] But to remain financially viable, an obstetric unit—staffed with a doctor, anesthesiologist, and several support nurses to safely perform emergency caesarean sections—requires about 200 births per year.[36] The share of rural counties with obstetric units declined from 75% in the 1980s to 40% in 2018.[37] Rural areas that lost maternity wards have seen more out-of-hospital and preterm births, along with a lower portion of deliveries involving C-sections.[38] Overall, however, maternity ward closures have led to a slight reduction in maternal morbidity because they have forced mothers to travel to higher-volume hospitals,[39] which tend to have improved infant and maternal outcomes.[40]
Prior to closures, rural hospitals furnished little inpatient care, but they were a key source of emergency care.[41] Rural residents use 50% more emergency hospital care than those in urban areas because of a shortage of primary-care providers. But rural emergency visits result in admission half as often as in non-rural areas.[42]
Rural areas already find it harder to access emergency care. Whereas 84% of Americans live within an hour of a Level 1 or 2 Trauma Center, only 24% of rural residents do.[43] This contributes to a 14% higher risk of death following traumatic injuries.[44] It also matters for other time-sensitive conditions, such as heart attacks, stroke, sepsis, burns, and neonatal care.[45]
In urban areas, hospital closures have little effect on the distance that patients travel to hospitals or on mortality rates associated with time-sensitive medical conditions.[46] But rural hospital closures are associated with a 9% increase in mortality, with significant mortality increases due to sepsis and stroke, in the affected service area.[47]
Rural emergency-department closures also increase mortality rates at nearby hospitals, which must absorb increased patient loads despite typically not being significantly higher in quality than the facility that closed.[48] These closures also force patients to travel longer for care, with ambulance transportation times increasing from an average of 14.2 to 25.1 minutes in areas experiencing hospital closures.[49] Although the rise in mortality at nearby hospitals declines over time—as they expand capacity to cover the strain—the harm due to lengthened travel time endures.[50]
Hospital closures have other negative effects on rural areas. Each closure, for example, leads to persistent declines in the local supply of physicians, across multiple specialties, including primary care,[51] as well as to an average loss of 220 jobs.[52] However, closures do not lead to a multiplier effect on employment outside the health-care sector—likely because non-health-care employment declines typically precede hospital closures.[53]
Assistance for Rural Hospitals
Rural hospitals are, and have long been, dependent on public payers.
Medicare accounts for 53% of discharges at rural hospitals, compared with 45% at urban facilities.[54] At urban hospitals, profit margins from privately insured patients averaged 35% in 2019—while, at small rural hospitals, that margin was, on average, only 3%.[55] Because 35% of rural hospitals are publicly owned (compared with 13% in urban areas), their survival owes much to state grants and local tax revenues.[56]
In 1946, Congress enacted the Hospital Survey and Construction (Hill-Burton) Act to increase hospital capacity in poor rural areas. It distributed funds in inverse proportion to regions’ number of hospital beds, yielding a substantial expansion of nonprofit and public hospitals—particularly in the South.[57]
When it established Medicare in 1965, Congress originally paid hospitals according to whatever reasonable costs they incurred in delivering care to eligible beneficiaries. This caused a major expansion of hospital capacity nationwide, as facilities were initially able to secure reimbursement for whatever capital investments they made.[58]
In 1982, Congress reined in the growth of expenses by ending cost-based reimbursement and instead fixing a schedule of fees that Medicare would pay for various medical procedures.[59] Aside from minor adjustments for factors such as geographic variations in labor costs, Medicare would subsequently pay different hospitals the same amounts for the same procedures. This led to increased profitability for efficient urban and suburban hospitals, while straining the finances of low-volume rural hospitals.
Congress has since established a variety of special provisions, such that 95% of rural hospitals now receive Medicare payments above standard national rates.[60]
In 2022, out of 4,650 Medicare-participating hospitals, 733 received higher payments as Medicare Dependent Hospitals (MDH), Sole Community Hospitals (SCH), or Low-Volume Hospitals (LVH).[61] These payments blend standard fee-schedule payments with previous reimbursements based on facility-specific costs, adjusted for inflation, and include bonuses for declining patient volumes.
In 1997, Congress established Critical Access Hospital (CAH) status to altogether exempt hospitals from standardized fees, and allow them to claim reimbursement of 101% of reasonable costs for inpatient, outpatient, and post-acute care. Unlike MDH, SCH, or LVH facilities, CAHs necessarily receive higher payments when the cost of the care they deliver increases.
CAHs must maintain a 24/7 emergency department and patient transfer agreements with hospitals with better capabilities. They must have no more than 25 beds and be located more than 35 miles from the nearest hospital. Prior to 2006, states could waive these distance requirements for facilities they deemed “necessary providers”—and such facilities have subsequently been permitted to retain that status.
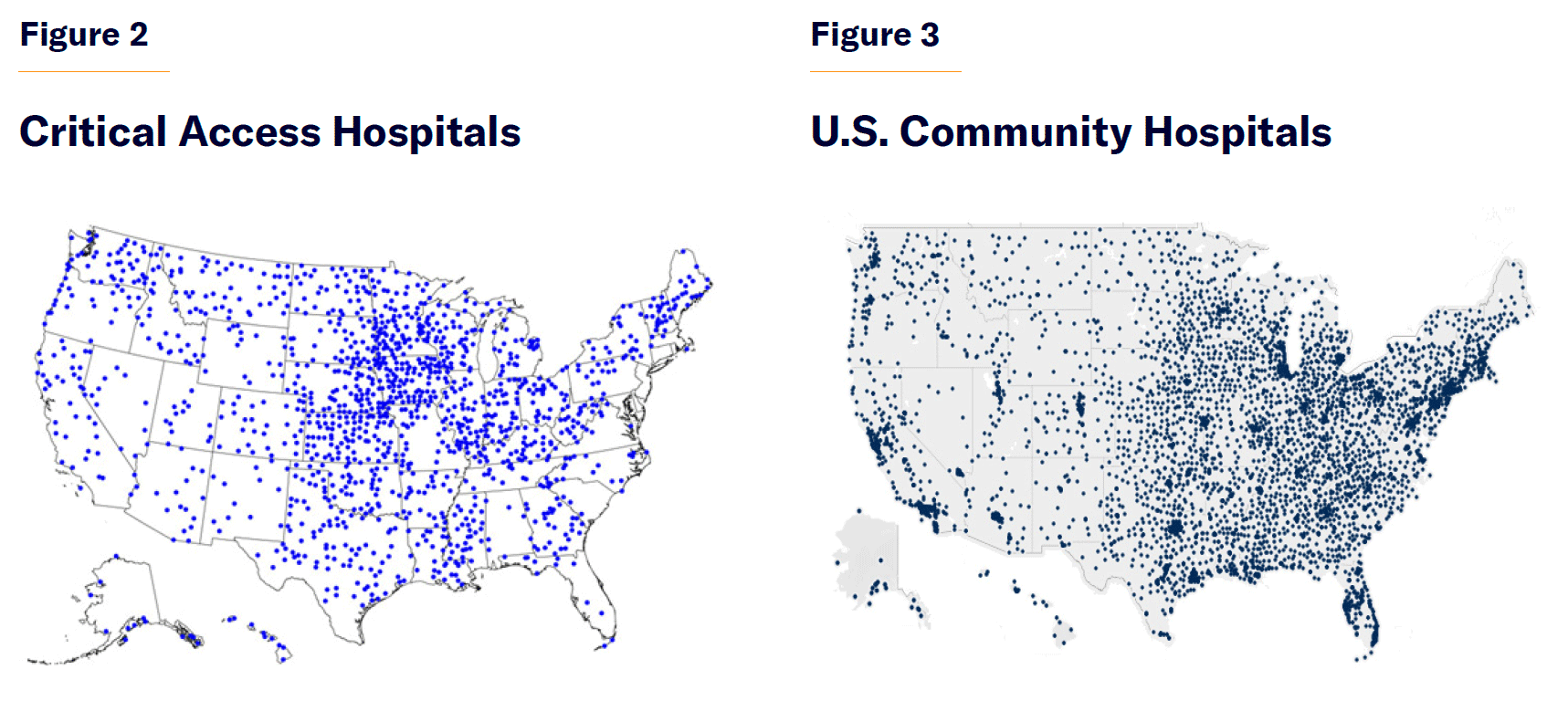
In 2022, 1,350 Medicare-participating hospitals had been classified as CAHs—80% of which were located less than 35 miles from another source of emergency care.[62] CAHs are concentrated in midwestern states. There are 82 in Iowa, 83 in Kansas, and 76 in Minnesota, but only 3 in South Carolina, 6 in Alabama, and 8 in Virginia (Figures 2 and 3).[63]
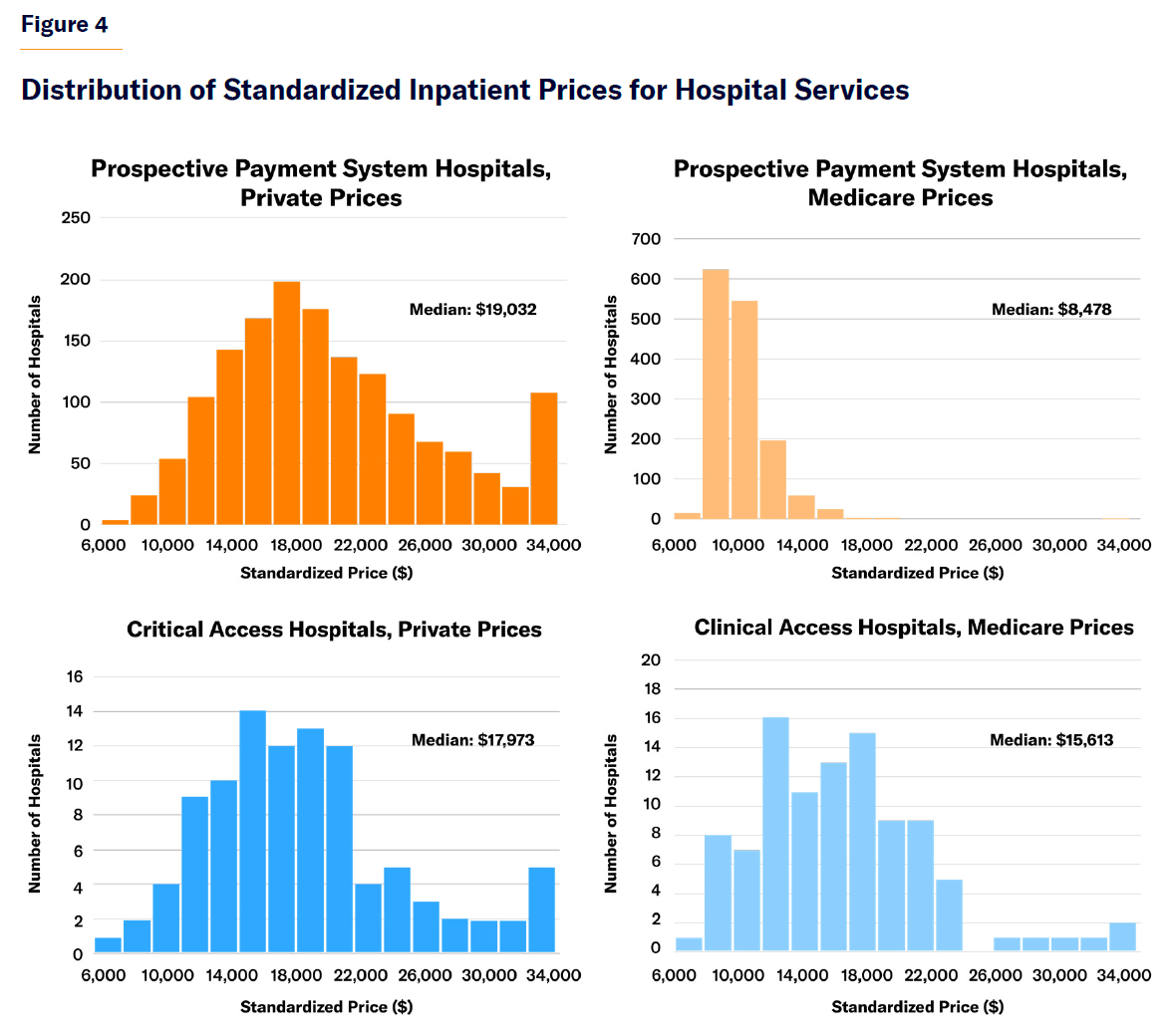
Critical Access Hospitals are paid similarly to other hospitals by private insurers. But whereas Medicare pays other hospitals much less than private insurance, it pays CAHs about the same as private insurers do. As a result, Medicare on average pays CAHs much more than it does other hospitals, with some CAHs being paid four times as much as standard Medicare rates (Figure 4).
The reestablishment of cost-based reimbursement at CAHs eliminated the most substantial incentives to control costs. Medicare payments to facilities go up when CAHs add labor and capital. From 1998 to 2002, payments per discharge at these facilities rose by 21%, while post-acute costs per day almost quadrupled.[64] Cost growth has compounded over time: the longer a hospital has been a CAH, the more its costs have grown.[65] By 2010, 83% of CAHs had MRI scanners.[66]
CAHs were less efficient than other rural hospitals, having more expenses and employees per inpatient admitted.[67] In 2014, Medicare paid CAHs an average of $2,000 per day for “swing beds” (which can be used either for acute or post-acute care)—almost four times the standard Medicare rate for skilled nursing facilities.[68]
In total, Medicare spent $12 billion on CAHs in 2022, amounting to only 6% of the program’s payments to hospitals.[69] MedPAC estimated that cost-based reimbursement led to $4 million more in Medicare fee-for-service payments to CAHs in 2022. This increase, they noted, alone exceeded CAH’s average all-payer profit of $1 million–$2 million.[70]
This increased spending on CAHs was an inefficient method of preventing hospital closures. A recent difference-in-difference analysis estimated that the conversion of 1,300 hospitals to CAH status averted the closure of only about 25 hospitals during the program’s first eight years. It concluded that increased spending did reduce mortality when directed to hospitals that “would have closed without the additional revenue” but that the “vast majority” of CAH funds went to facilities that would have remained open anyway.[71]
Wealthier communities tend to benefit more from cost-based Medicare payments because they have more lavish facilities (with 40% higher costs on average) and fewer uninsured local residents to support.[72] MedPAC has concluded that CAH status can distort competition, reduces incentives for cost control, favors wealthy communities, and doesn’t necessarily prevent closures.[73] CAHs within 15 miles of other hospitals are larger, better-quality, and financially stronger.[74] President Obama’s 2015 budget therefore proposed eliminating CAH designations for hospitals within 10 miles of other facilities.[75]
The CAH model is becoming increasingly unsustainable. To receive additional revenues from Medicare, CAHs must maintain the capacity to deliver inpatient care and all the costs that entails. But technological progress has diminished the recovery time associated with surgical procedures—reducing the need for lengthy inpatient stays and allowing them to be performed increasingly on an outpatient basis. CAHs have also seen inpatient volumes fall because of declining local populations and the increasing capital intensity of cutting-edge surgical procedures. Heart-attack patients are now routinely transported to facilities that offer angioplasty and cardiac surgery, while stroke patients are often helicoptered to larger specialized facilities.[76]
The average number of discharges per CAH fell from 624 in 2003 to 335 in 2016—fewer than one per day, thus increasing the burden of overhead costs on each discharge.[77] As one hospital leader noted of the CAH model: “You end up having a hospital that you have to staff for inpatient services, and you literally don’t have inpatient services.”[78]
The expansion of Medicaid to able-bodied adults did not significantly improve the financial situation of CAHs. Medicaid patients account for only a small share of CAH revenues, and they are not hugely profitable,.[79] CAHs in expansion states did not see expanded operating profit margins, increased staffing levels, or improved patient outcomes following pneumonia or heart failure.[80]
In recent years, the flow of subsidies to CAHs has been further squeezed by Medicare policies that are designed to forestall costly inpatient hospitalizations, such as Accountable Care Organizations or Medicare Advantage (MA). MA plans typically provide cost-based reimbursement to CAHs according to Medicare’s standard terms, even though they are not legally required to do so.[81] But they may require prior authorization for inpatient procedures, or steer patients to other hospitals that provide higher-quality care at lower cost.[82] Hospitals complain that this leaves them with substantially lower revenues from Medicare patients, who normally account for the largest portion of their revenues.[83] During 2013–23, the share of rural Medicare beneficiaries enrolled in MA increased from 18% to 44%.[84]
Reform Proposal
Attempts to prop up rural hospitals through cost-based reimbursement have driven up the cost of medical care, without truly assuring the continued availability of essential emergency services to communities. Tying assistance to hospitals to the volume of inpatient care that they deliver does not help facilities that are most in need because their inpatient volumes have collapsed. Nor is this approach compatible with Medicare reforms that attempt to promote cost-efficiency in the procurement of medical care.
In 2016, MedPAC recommended a new system of public subsidies to directly support emergency care at geographically isolated rural hospitals, while encouraging fewer time-sensitive services (such as MRIs) to be delivered by lower-cost providers.[85] Congress took up this recommendation in the Consolidated Appropriation Act of 2021, by establishing the Rural Emergency Hospital (REH) model.[86]
From 2023, Rural Emergency Hospitals were each entitled to regular lump-sum payments from the Medicare program ($3.2 million that year, subsequently indexed for inflation), regardless of their inpatient volume.[87] This payment is equal to the average overpayment to CAHs relative to what Medicare would normally have paid them for medical services. REH facilities are also paid at 105% of Medicare rates for hospital outpatient services and at standard rates for post-acute care.[88] Medicare-participating hospitals can claim REH “facility payments” if they maintained an emergency department staffed 24 hours per day; provide laboratory, diagnostic, pharmacy, and discharge planning services; and establish a transfer agreement with a top trauma center. These facilities also must have fewer than 50 beds and have an average patient length of stay of less than 24 hours in order to qualify for REH payments.[89]
Although 1,569 rural hospitals are eligible to convert to REH status, only 32 hospitals signed up in the program’s first 18 months.[90] This take-up is slow but nonetheless exceeds the typical number of rural hospital closures over the same period.[91]
Congress took a step in the right direction by establishing the REH model. The program helps hospitals maintain essential services without forcing patients to overpay for poorer-quality elective care.
However, even as federal subsidies for rural CAHs are increasingly being squeezed by Medicare Advantage, few rural hospitals have opted for conversion to REH status. This suggests that the inability of rural hospitals to maintain their current business model is often exaggerated.
One obstacle to REH conversion is that it requires supportive state legislation. States should authorize REH payment arrangements and reform Certificate of Need laws to permit hospitals to reorganize as emergency-care-centric institutions. They should also adjust Medicaid payments to hospitals to accommodate the REH business model.
Congress should also reform the REH model itself to make it easier for hospitals to convert. It can be a huge challenge for small rural hospitals to transform from inpatient providers to emergency-focused outpatient institutions, as they often lack the administrative capacity and access to capital (through equity finance, borrowing, donations, or retained earnings) to finance major restructuring.
To facilitate conversion, Medicare should allow hospitals to claim three years of REH lump-sum payments up front, if they commit to conversion to REH status for five years. This would greatly facilitate the transition process, by allowing them to fund one-time administrative and construction expenditures that are associated with conversion.
Hospitals could use up-front REH support payments to remodel emergency departments, purchase new equipment, or retrain staff. These payments could also be used to support the development of improved ambulance capacity for transfers to nearby trauma centers and facilities capable of high-quality surgical procedures.
The front-loading of REH payments would not impose substantial additional costs on federal taxpayers because it would merely shift expenditures within a predefined five-year window.
Although reformed REH support payments may appeal disproportionately to hospitals for which CAH status is relatively less lucrative, these additional costs would likely be offset by reduced public expenditures on non-Medicare patients.
Rural Americans are already willing to travel to receive better-quality medical care at lower cost. Aiding rural hospitals by allowing them to charge more for Medicare patients therefore often fails to ensure the continued viability of essential emergency care—and it may be leading to poorer inpatient care for rural patients. Congress was therefore right to offer focused support for hospitals to provide emergency care. They should make it easier for isolated rural hospitals to claim more of these payments up front, so that these facilities are able to finance the changes needed to focus on emergency care.
Endnotes
Photo: Althom / iStock Editorial / Getty Images Plus
Are you interested in supporting the Manhattan Institute’s public-interest research and journalism? As a 501(c)(3) nonprofit, donations in support of MI and its scholars’ work are fully tax-deductible as provided by law (EIN #13-2912529).

















