One of the key themes I’ve tried to illustrate throughout this publication is that chronic illness has vastly increased over the last 150 years. Furthermore, again and again, doctors of each generation who observed each successive wave of that increase noticed that the treatments they learned at the start of their careers were much less effective for treating the patients they saw at the conclusion of their careers.
For example, here recent article, I discussed this collective loss of vitality in more detail, and listed what I believed were the primary culprits (which has been quite a challenge as there are now so many unhealthy things in our environment). In addition to listing the key culprits many are familiar with (e.g., the vaccination program has had a horrific impact on our health), I proposed another primary cause of chronic illness was modern life being highly disruptive to the natural rhythms the body depends upon for self-regulation and self-repair.
I believe this concept is relatively under appreciated within Modern Medicine (Allopathy) because, unlike almost any other medical system in history, our scientific approach to understanding the body does not recognize the concept of an innate “health” of the body, and as such, many Allopathic treatments are based around doing what they can to stabilize (e.g., in the ICU) or alter the body (e.g., through a surgery) and then hoping the body eventually works things out from there. In contrast, most other medical systems focus on what can be done to augment this innate capacity for recovery (health) and trust that through doing so, the present issue will resolve itself.
Note: typically the Allopathic approach (forcing the body to assume the state deemed necessary for the patient) is ideal to utilize for acute conditions, whereas the health-augmenting approach is what gets the best results for chronic conditions (something Allopathic medicine is well-known for struggling with).
At this point, I believe there are three reasons why we utilize the Allopathic model (discussed further here) rather than the health-focused model:
• The Allopathic model lends itself to creating a large number of perpetual treatments and diagnostic services for each person. Because this is so lucrative, it inevitably incentivizes its proponents to monopolize the entire medical market and healthcare practitioners to prioritize creating and utilizing its therapies.
• One of the fundamental psychological neuroses that exists in our culture is the need to control things and believe one knows exactly what’s happening. Because of this, our culture tends to default towards adopting methods and models that dominate nature rather than working in harmony with it and refusing to accept the inherent uncertainty that trusting in the path nature takes entails. Trusting in the health of the body to cure illness hence is opposed to the cultural philosophy Allopathy emerged from.
• Knowing if a therapy actually “works” is quite challenging, especially if the change can only be observed over a long time. Because of this, most medical research is based on whether an overt change can be consistently observed within a patient (e.g., lowering their blood pressure) and hoping that change will yield a long-term benefit rather than evaluating the long-term prognosis of people who receive a medical intervention. Because of this, medical research is strongly biased towards evaluating treatments that create an overt change (e.g., pharmaceutical drugs) rather than ones that augment the body’s health and lead toward a gradual recovery. Likewise, it is much easier to diagnose someone by their symptoms (and prescribe drugs to treat those symptoms) than it is to identify the root cause of their disease.
Self Regulating Cycles
The “health” of the body is highly dependent on the normal functioning of a variety of repeating cycles that occur within it.
For example:
• Practicing slow, smooth, and expansive nasal breathing has a profound impact on one’s health and longevity because breathing regulates many different critical physiologic functions.
• Normal exposure to sunlight serves a variety of critical functions for health, and once it is lost, one’s risk of dying doubles, and a variety of other conditions, such as depression set in (discussed further here).
• People need regular physical activity, whereas once they become sedentary, a variety of significant health issues arise. In turn, we have all noticed individuals who make a point to walk daily have dramatically improved longevity.
• The mind is designed to alternate between periods of rest and activity. Yet, in our modern era, we have to think constantly, which often occurs in conjunction with significant stressors.
• Humans are meant to alternate between periods of eating and not eating (fasting) rather than continually eating.
In short, many of the natural rhythms our bodies rely upon for self-regulation are heavily disrupted in modern society, which in turn results in a variety of consistent derangements to normal physiology that are now seen throughout the population.
Note: based on how much we frequently see people’s health improve once they restore their natural rhythms, I now believe their disruption is a primary cause of the widespread health dysfunction we see now.
The Importance of Sleep
Throughout my career, I’ve met countless integrative practitioners who believed that one of the most important things to do when treating a chronic illness is to normalize their patient’s sleep, as this cyclical process is one of the foundational methods the body uses to restore its health. Unfortunately, patients with chronic illnesses tend to have highly disrupted sleep cycles which are often very challenging to correct (e.g., insomnia is fairly common following a COVID-19 vaccine injury).
The important thing to understand about sleep is that it is a tightly regulated cycle which is both highly responsive to signals from the environment and also responsible for maintaining many of the other critical rhythms within the body.
During sleep, the body cycles through different phases of sleep, each of which performs a critical function (e.g., deep NREM sleep heals the brain and allows toxins to drain out of it through the glymphatics, while REM sleep consolidates memories and allows one to process the emotions of their experiences). A typical sleep cycle goes as follows:
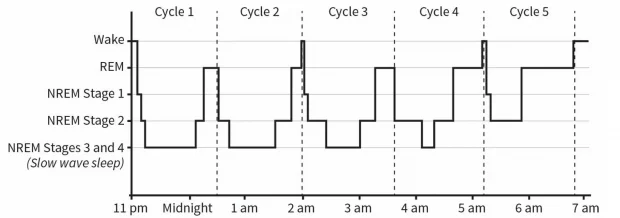
Note: since REM sleep predominates later at night, not sleeping long enough disproportionately disrupts REM sleep.
Matthew Walker is one of the world’s most vocal sleep researchers. In his book Why We Sleep, he argues that some of the most important functions of sleep include:
- Maintaining circulatory health and preventing heart attacks.
- Ensuring proper metabolic health (e.g., sleep deprivation causes hunger, diabetes, and weight gain).
- Ensuring proper immune function (e.g., you are more likely to get the flu if you are sleep deprived).
- Preventing cancer.
- Preventing fatigue and brain fog (which are typically the most overt symptoms we notice from sleep deprivation).
- Remaining awake and alert.
- Healing and restoring the brain (e.g., Alzheimer’s disease is strongly linked to poor sleep).
- Regulating hormonal function and maintaining fertility (e.g., sleep deprivation lowers testosterone levels).
- Processing emotional trauma (e.g., sleep is typically disrupted in PTSD, and PTSD often significantly improves once a drug is given which prevents PTSD from disrupting sleep).
- Integrating one’s sense of reality and accurately interpreting emotional signals from one’s environment.
- Sleep allows the rational mind (the prefrontal cortex) to control counterproductive impulses (e.g., emotional outbursts, or binge eating).
- Maintaining one’s mental health (e.g., it’s well known that a variety of psychiatric conditions, such as bipolar episodes are triggered by periods of sleep deprivation).
- Maintaining one’s sense of reality (e.g., prolonged sleep deprivation can trigger psychosis, and sleep is known to be disturbed in schizophrenic patients).
- Facilitating creativity (e.g., many paradigm-shifting discoveries came from dreams, Thomas Edison was well-known for using dreams to concoct his inventions, and when people are woken up from REM sleep, they often demonstrate a radically improved abstract problem solving capacity).
- Reducing one’s sensitivity to pain (whereas sleep deprivation increases it).
- Facilitating the long-term retention of memories.
I generally agree with this list (and will cite more studies supporting it later in the article). Likewise, I am sure many of know firsthand how bad you feel when you are sleep deprived. Here are some of my personal experiences with sleep:
•I am fairly sensitive to the baselines within my body and I immediately notice that things within me go awry if I’ve had insufficient sleep. For example, I notice impairments in a variety of neurologic functions (e.g., I become significantly less able to tolerate the cold, my coordination worsens, and it’s much harder for me to maintain my focus in either an intellectual or social task).
•During periods of significant sleep deprivation, I will notice I have fleeting pain within the heart muscle and periodic arrhythmias. This is corroborated by a study that found one night of modest sleep reduction (as little as one or two hours) quickly increased one’s heart rate and blood pressure.
•During periods of insufficient sleep, I experience general mental fogginess that persists until I get a good night’s sleep (and sometimes two).
•I have repeatedly observed that one’s recovery from a traumatic brain injury is highly dependent upon whether they get significant sleep after the incident, something I in part attribute to improved venous and lymphatic drainage (e.g., most glymphatic drainage occurs during NREM sleep and when you are lying down, there is much greater venous drainage than while standing). Likewise, research shows that a significant part of the gradual recovery from strokes occurs while sleeping.
•Before high school, I accidentally figured out how to use sleep to facilitate the long-term retention of information. This “lifehack” allowed me to memorize large volumes of information in very little time, and was the main reason I was able to get through the academic system while simultaneously teaching myself a separate curriculum (e.g., I spent more time studying things I was not assigned to learn during medical school than the material I was expected to learn). I mention this because the rules I discovered through experimenting with my “lifehack” matched what Walker’s own data demonstrated (although some of them also went beyond the scope of what Walker looked at).
Note: NREM sleep is responsible for eliminating unnecessary memories, whereas REM sleep processes the day’s experiences and reinforces them into long-term memory.
•I tend to gain weight during periods of poor sleep.
Finally, Walker cites many examples of severe consequences occurring after prolonged periods of significant sleep deprivation (e.g., death or psychosis). I have also seen similar things occur. For instance, periodically I will have a patient who comes to me after engaging in an unsafe spiritual practice which involved staying awake for multiple days, after which they developed a permanent psychiatric or spiritual disorder (discussed further here).
Quantifying the Importance of Sleep
Any individual, no matter what age, will exhibit physical ailments, mental health instability, reduced alertness, and impaired memory if their sleep is chronically disrupted.
Even when controlling for factors such as body mass index, gender, race, history of smoking, frequency of exercise, and medications, the lower an older individual’s sleep efficiency score, the higher their mortality risk, the worse their physical health, the more likely they are to suffer from depression, the less energy they report, and the lower their cognitive function, typified by forgetfulness.
Immunity
During periods of sleep deprivation, immune system function significantly decreases. Some of the consequences of this include:
Cancer—Numerous studies have found an association between sleep deprivation and cancer (while conversely, others have not—which I believe is due to the difficulty of properly studying this topic). Data supporting the link includes:
•In 2010, using all the available evidence, the WHO classified shift work (one of the most reliable ways to heavily disrupt natural sleep cycles and something many workers in the healthcare field experience) as a probable human carcinogen. This link is also supported by a 2023 review paper.
• An English study of 10,036 people over 50 found that poor sleep resulted in a 33-62% increased risk of cancer.
• A study of 23,620 Europeans found that those who slept for less than 6 hours per day were 43-46% more likely to develop cancer.
• When mice were intentionally sleep deprived, they experienced their speed and size of cancer growth roughly doubled, relative to the well-rested group.
• When healthy young men slept for four hours, compared to nights where they slept eight hours, there was a 72% decrease in their circulating natural killer cells (which are responsible for eliminating cancers).
• Two different studies found sleep apnea (which disrupts healthy sleep) caused a large increase in one’s risk of dying from cancer.
• Existing data shows that sleeping pills (which disrupt normal sleep) are associated with a large increase in one’s risk of cancer.
Note: the increased cancer risk from poor sleep may also be due to disturbances in the body’s normal release of melatonin or insufficient tissue oxygenation.
Infections—individuals who are sick are more likely to develop infections (e.g., most times I get sick are after periods of prolonged poor sleep). Some of the evidence to substantiate this common observation includes:
• Rats that are not allowed to sleep deteriorate and eventually die. When death occurs, it is typically due to sepsis from their gut bacteria.
Note: humans also can develop blood infections from their gut bacteria, but it typically requires circumstances that predispose them to it (e.g., on a central venous catheter as that provides a site bacteria in the blood stream can adhere to, or following a bowel rupture).
• A study determined how much sleep research subjects had had in the last week and then exposed them to the common cold virus (by squirting it in their nose). It found those who had averaged less than 7 hours of sleep were 2.94 times more likely to develop a cold than those who had more than 8 hours. It also found those with poor sleep efficiency (how much of the time bed you are asleep) were 5.50 times more likely to develop a cold than those with good sleep efficiency.
A study of 56,953 nurses found women who slept 5 hours or less were 1.7 times as likely to develop pneumonia over a 4-year period compared to those who slept 8 hours a night.
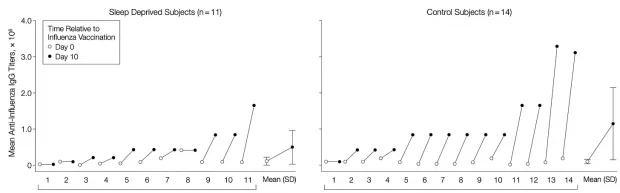
• A 2002 study compared 14 healthy young men who slept for 7.5-8.5 hours a day to 11 others who restricted their sleep to 4 hours a night for 6 days, after which all 25 received a flu shot. The sleep-deprived group was observed to produce less than half the vaccine antibodies seen in the control group, and this loss continued after normal sleep had been restored
Note: this association has also been seen with other influenza vaccines along with hepatitis A and B vaccines.
• When patients take sleeping medications that interfere with the sleep cycle, they have a significantly increased rate of infections (e.g., one large study found they increased one’s risk of pneumonia by 54% and one’s risk of dying from pneumonia by 32%).